Write an article about
Five patients (3 men and a couple of women) with unilateral craniofacial fibrous dysplasia were admitted to the Department of Oral and Craniomaxillofacial Surgery on the Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, from January 2020 to June 2020. The average age was 29 years old (range 18–54 years old). The patients’ characteristics and demographics are thoroughly described in Table 1.
Table 1 Patient information.
All medical practices followed the Declaration of Helsinki on medical protocols. This study was approved by the Shanghai Ninth People’s Hospital Institutional Review Board (approval number SH9H-2019-T142-1). All methods were performed in accordance with the relevant guidelines and regulations of our hospital. Informed consent was obtained from all of the participants. Informed consent has been obtained to publish the data and pictures in a web based open-access publication.
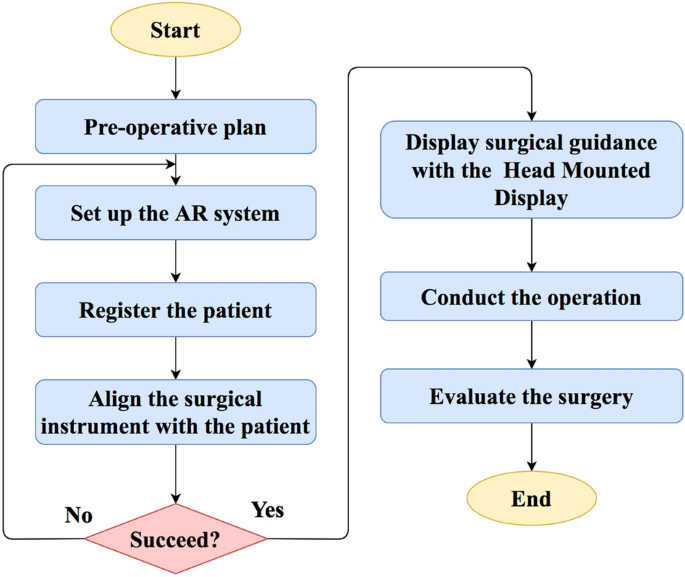
AR-assisted facial recontouring of patients was performed by applying the next workflow, which was implemented by surgeons and biomedical engineers, as shown in Fig. 1.
Figure 1
The workflow of the system.
STEP 1: preoperative operation plan
A computed tomography (CT) (GE Healthcare, Fairfield, USA) scan was performed pre-operatively, after which the CT images were configured in Digital Imaging and Communications in Medicine (DICOM) format and imported into planning software (ProPlan 2.1, Materialise NV, Leuven, Belgium) to generate a 3D craniomaxillofacial model. For a more accurate placement of the teeth, the dental stone model was scanned with a high-resolution laser surface scanner (Smart Optics AS, Bochum, Germany), yielding a digitalized dental model that may then be merged into the 3D skull model. At this point, we obtained a computerized merged model interpreting highly accurate dental and bony elements17. Cranial anatomy was assessed in 3D views and multiple planes (axial, coronal, and sagittal). The normal anatomical contour of the deformed region was mimicked from the conventional contralateral side through the mirroring function based on the median sagittal plane as a reference to find out the quantity of bone lesion to be removed.
STEP 2: setup of the AR system and registration
The setup of the AR system consisted of various essential parts for preparation of an integrated image: Head Mounted Display (Hololens, Microsoft Corporation, USA), workstation and optical tracking system (Northern Digital Inc., Ontario, Canada). Figure 2 illustrates the connection between the various components and system registration, as described below.
Figure 2
Configuration of the proposed AR navigation system: (a) digital reference frame fixed to the patient’s craniofacial skeleton; (b) surgical drill with clamped digital reference frame; (c) optical tracking system and workstation; (d) Head Mounted Display; (e) 3D virtual planning and the position of surgical drill.
A digital reference frame (DRF) firmly fixed to the patient’s craniofacial skeleton will be tracked by the optical tracking system and the Head Mounted Display camera, and the surgical drill with one other clamped DRF will be tracked by the optical tracking system. The workstation is used to process and update the information of the surgical drill and the patient’s craniofacial skeleton’s 3D location and to transfer the information to the Head Mounted Display. The Head Mounted Display mainly played a task in visualizing the hologram, and the 3D virtual planning and the position of surgical drill are displayed through the Head Mounted Display for an intraoperative guidance.
STEP 3: intraoperative guidance with augmented reality
After the registration step, the surgeon performs the surgery wearing the Head Mounted Display. Following the exposure of the dysplastic zygomaticomaxillary bone, the dysplastic bone was shaved using the surgical drill. With the help of the AR navigation system, the surgeon can directly visualize the craniofacial skull and lesion images, surgical field and extra information reminiscent of the position of the surgical drill in real time through the pinnacle mounted display (Fig. 3). More importantly, the AR system not only ensures that the contouring drill is positioned within the surgical field for bone contouring but additionally enables statement of mass resection in real time. Therefore, the surgeon can provide continuous feedback and review the recontouring procedure intraoperatively in keeping with the virtual design. Figure 4 illustrates the precise instrument-based image-guided recontouring procedure guided by real-time visualization through the pinnacle mounted display.
Figure 3
Surgeon carrying out the operation wearing the pinnacle mounted display.
Figure 4
Different stages of the intraoperative guidance: (a) When the drill remains to be at a big distance from the designed surface (> 1 mm), the model is rendered in green, and real-time data will likely be displayed. (b) When the drill is about to achieve the designed surface (≤ 1 mm), the model is rendered in red, and real-time data will likely be displayed.
The different stages of intraoperative real-time guidance are as follows:
-
1.
When the drill remains to be at a big distance from the designed surface (> 1 mm), the model is rendered in green, and real-time data will likely be displayed;
-
2.
When the drill is about to achieve the designed surface (≤ 1 mm), the model is rendered in red, and real-time data will likely be displayed.
STEP 4: Evaluation of accuracy of the AR system
CT scanning was performed 3 days following surgery. The accuracy of the surgery was assessed by superimposing the post-operative 3D craniomaxillofacial model onto the pre-operative virtual plan. The detailed evaluation procedure is as follows:
The pre-operative virtual plan and post-operative 3D craniomaxillofacial models are aligned in a standard coordinate space. A program was designed using VTK (The Visualization Toolkit, Kitware, Inc., USA) to align the models. By choosing the paired points on the unchanged region of the skull, the planned model’s coordinate space was transformed into that of the post-operative model via point cloud matching. Next, each models were imported into 3D evaluation software (Geomagic Control X, 3D Systems Inc., South Carolina, USA) to analyse the superimposed discrepancy. Hundreds of pairs of points were generated uniformly within the surgical area, and the position of every point was obtained, as shown in Fig. 5. Each of the paired points was positioned along the conventional vector of the skull surface. The distance between the paired points indicated the surgical discrepancy.
Figure 5
The accuracy evaluation for the performance of the system: The pre-operative virtual plan and post-operative 3D craniomaxillofacial models were imported into 3D evaluation software (Geomagic Control X, 3D Systems Inc., South Carolina, USA), and tons of of pairs of points were generated uniformly within the surgical area. Each of the paired points was positioned along the conventional vector of the skull surface. The distance between the paired points indicated the surgical discrepancy.
make it easy to read for teens.Organize the content with appropriate headings and subheadings (h1, h2, h3, h4, h5, h6) and made content unique. Include conclusion section and don’t include the title. it must return only article i dont want any extra information or introductory text with article e.g: ” Here is rewritten article:” or “Here is the rewritten content:”